Managing Tardive Dyskinesia Movements
Tardive dyskinesia, a distressing neurological condition linked to certain medications, notably affects facial muscles and limbs with involuntary movements. It necessitates a multifaceted management approach encompassing both pharmacological and non-pharmacological strategies. Understanding diagnosis, prevention, and the role of healthcare providers enhances patient care and improves outcomes for individuals facing this chronic condition.

Tardive dyskinesia affects thousands of individuals worldwide, creating challenges that extend beyond the physical symptoms to encompass social, emotional, and practical aspects of daily living. The condition manifests through various involuntary movements, including facial grimacing, tongue protrusion, lip smacking, and rhythmic movements of the arms, legs, or trunk. These symptoms can range from mild and barely noticeable to severe and debilitating, making effective management crucial for maintaining independence and well-being.
Understanding Tardive Dyskinesia and Its Impact
The development of tardive dyskinesia involves complex changes in brain chemistry, specifically affecting dopamine receptors in areas responsible for movement control. Unlike other movement disorders, tardive dyskinesia often emerges after months or years of medication exposure, making early detection challenging. The condition can persist even after discontinuing the triggering medication, though some cases may improve over time with appropriate intervention.
The impact extends beyond physical symptoms, affecting communication, eating, social interactions, and professional activities. Individuals may experience embarrassment, social withdrawal, and decreased quality of life. Understanding these broader implications helps healthcare providers and families develop comprehensive support strategies that address both medical and psychosocial needs.
Treatment Options and Management Strategies
Effective management of tardive dyskinesia requires a multifaceted approach tailored to individual circumstances. The primary strategy involves evaluating the necessity of continuing causative medications while weighing the risks and benefits. In some cases, switching to alternative medications with lower tardive dyskinesia risk may be appropriate.
VESA inhibitors, specifically valbenazine and deutetrabenazine, represent FDA-approved treatments specifically designed for tardive dyskinesia. These medications work by reducing dopamine signaling in brain areas controlling movement. Clinical studies demonstrate significant symptom reduction in many patients, though individual responses vary.
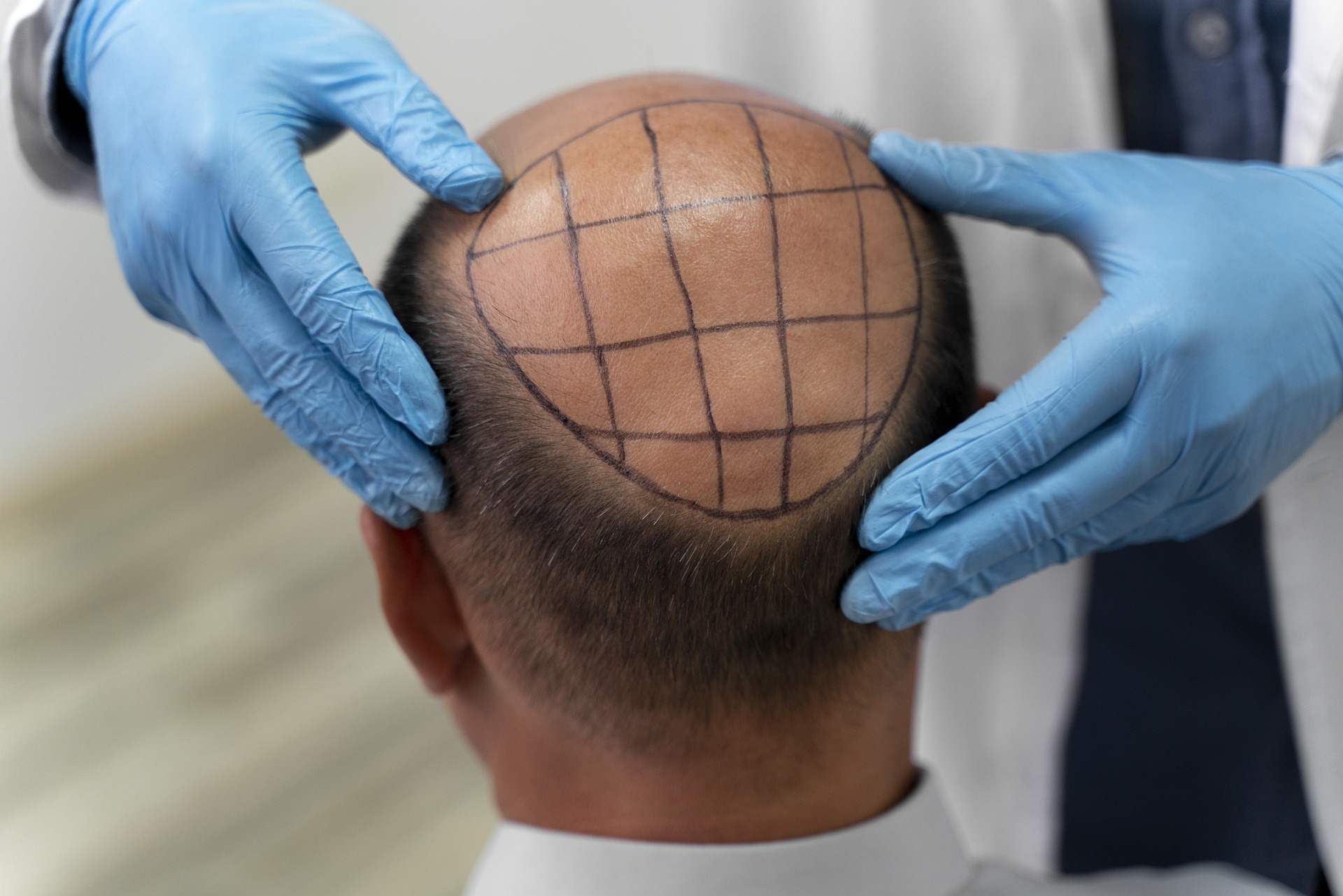
Additional treatment approaches include botulinum toxin injections for localized symptoms, particularly facial or neck movements. Physical therapy and occupational therapy can help maintain mobility and develop adaptive strategies for daily activities. Some patients benefit from complementary approaches such as yoga, tai chi, or meditation to manage stress and improve overall well-being.
Role of Healthcare Providers in Monitoring and Diagnosis
Healthcare providers play a crucial role in early detection and ongoing management of tardive dyskinesia. Regular monitoring using standardized assessment tools like the Abnormal Involuntary Movement Scale (AIMS) helps identify emerging symptoms before they become severe. This systematic approach enables timely intervention and treatment modifications.
Neurologists, psychiatrists, and primary care physicians must collaborate to balance mental health treatment needs with movement disorder risks. Regular medication reviews, dose adjustments, and consideration of alternative treatments form essential components of comprehensive care. Patient education about symptom recognition empowers individuals to report changes promptly.
Documentation of baseline movement patterns before starting high-risk medications provides valuable reference points for future assessments. Healthcare teams should establish clear protocols for monitoring frequency and intervention thresholds to ensure consistent, proactive care.
Prevention and Risk Management
Prevention strategies focus on minimizing exposure to high-risk medications while maintaining effective treatment for underlying conditions. When antipsychotic medications are necessary, using the lowest effective dose for the shortest duration reduces tardive dyskinesia risk. Newer atypical antipsychotics generally carry lower risk compared to older typical antipsychotics.
Regular movement assessments should begin before starting high-risk medications and continue throughout treatment. Early detection allows for prompt intervention, potentially preventing symptom progression. Risk factors including age, gender, diabetes, and substance use history should inform monitoring frequency and treatment decisions.
Patient and family education about tardive dyskinesia signs enables early reporting of symptoms. Clear communication about risks and benefits helps individuals make informed decisions about their treatment options while understanding the importance of adherence to monitoring protocols.
| Treatment Option | Provider Type | Estimated Monthly Cost |
|---|---|---|
| VESA Inhibitors (Valbenazine) | Neurologist/Psychiatrist | $3,000-$5,000 |
| Botulinum Toxin Injections | Movement Disorder Specialist | $500-$1,500 |
| Physical Therapy | Licensed Physical Therapist | $200-$400 |
| Occupational Therapy | Occupational Therapist | $150-$350 |
| Specialist Consultations | Neurologist | $300-$600 per visit |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Why You Should Learn More About Tardive Dyskinesia Today
Staying informed about tardive dyskinesia developments benefits patients, families, and healthcare providers alike. Research continues to advance understanding of the condition’s mechanisms and treatment options. New medications, therapeutic approaches, and management strategies emerge regularly, offering hope for improved outcomes.
Education empowers individuals to advocate for appropriate care, recognize symptoms early, and make informed treatment decisions. Understanding available resources, including support groups, patient assistance programs, and specialized care centers, helps navigate the healthcare system effectively.
Early intervention and comprehensive management can significantly improve outcomes and quality of life. By staying informed about tardive dyskinesia, individuals can work collaboratively with healthcare providers to develop personalized treatment plans that address their specific needs and circumstances while minimizing the impact of this challenging condition.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.